Health Center Home
Metabolism 101: The basics for weight management
What is metabolism?
Metabolism is the biochemical process of combining nutrients with oxygen to release
the energy our bodies need to function. Metabolism is typically measured in kilocalories or,
more commonly, calories. Total energy expenditure (TEE) represents the calories needed for
maintaining body functions, daily activity (occupational end lifestyle), and the energy cost exercise or planned activity.
What is resting metabolic rate?
Resting metabolic rate (RMR) represents the calories that the body burns each day
to maintain vital body functions (e.g., heart rate, brain function, breathing, etc.).
In simple terms, it is the number of calories a person would burn if they were sitting in
a chair all day long doing nothing. An individual?s RMR is approximately 75% of their TEE
and the remaining amount (i.e. estimated 25%) is attributed to daily activity [1].
Why is metabolism unique to each individual?
Metabolism is influenced by a number of factors, such as; bodyweight, muscle weight, age, gender,
and hormones. Muscle burns more calories than fat; an individual with more muscle will have a higher
metabolism. In an example from a scientific study is provided in figure 1. Individuals with similar
physical characteristics (i.e., bodyweight, gender, age, etc.) can have large differences -900 calories
per day [2]. This may explain why weight loss varies among similar individuals participating in the same weight loss program.
Metabolism declines naturally in adults at a rate of about 2 to 10% per decade after the age of 25 years.
This decline is the result of decreased muscle weight. To minimize this decline, individuals can build or
maintain muscle weight through strength training.
Men normally have higher metabolic levels than women due to men having more muscle weight.
Certain hormones (e.g., testosterone) can also increase or decrease metabolism. Estimates can not
account for individual variability, pre-existing medical conditions, and medications needed to help
control various illnesses or chronic diseases. Patient?s taking blood pressure lowering medications may
experience a decrease in metabolism by as much as 15%. Patient?s taking some anti-depressants may experience
a decrease in metabolism by as much as 20%. By measuring RMR, healthcare providers can ensure that the best and
most accurate nutritional care is provided and can positively influence individual results.
Weight Loss
It is common for metabolism to decrease following active weight loss. This should not be alarming
because the metabolic decrease is the result of tissue (i.e. fat and muscle) loss. Weight loss
ideally results in proportionately more fat loss and some muscle loss. Usually, if you lose 10 lbs of
bodyweight approximately 7 lbs of this weight loss is fat weight.
In addition, metabolism will decrease in response to consuming fewer amounts of calories. Most
individuals experience a change in metabolism without realizing it. Weight loss may be easy for the first
few pounds but becomes more difficult overtime.
Figure 1. RMR variability among women with similar physical characteristics. Foster et al. (1988).
At a lower metabolism, an individual must adjust their nutrition and/or activity level to lose additional weight.
However, following weight loss, metabolism may increase once an individual?s weight becomes stable.
During weight loss it is helpful to monitor changes in metabolism and make necessary nutrition adjustments for
successful weight management. A rule of thumb is to reassess your metabolism following every 10 to 15 lbs of weight loss.
Why is it necessary to measure metabolism?
Since metabolism accounts for a majority of the total calories a person needs each day, it is an important
component to establishing daily calorie needs, whether they are trying to lose or maintain bodyweight. Most healthcare
providers recognize metabolism can be altered due to a variety of circumstances such as illness or disease, medications,
genetics, and weight change. When managing daily nutritional needs, knowledge of RMR is important when adjusting calorie recommendations.
Traditionally, healthcare providers would not have access to RMR measurement technology and relied on estimates of metabolism.
Since metabolism is very different among individuals, estimating often leads to errors and can lead to in-accurate nutrition plans.
With in-accurate nutrition plans patients might follow a plan that causes weight gain or minimizes weight loss.
As technology advances, healthcare providers must reassess patient practice standards. The most accurate assessment
of calorie needs is measuring oxygen consumption that determines metabolism. Recently, the American Dietetic Association
issued clinical guidelines for developing daily nutrition plans and recommends healthcare providers measure metabolism in-place
of using estimates [3]. Developing an accurate nutrition plan from measured metabolism will eliminate guesswork for both the
healthcare provider and patient.
A study published in 2008, indicated better success when nutrition plans were developed from measured RMR.
From this study, the study participants experienced 50% more weight loss than those who had a nutrition plan
based from estimates (figure 2) [4]. The researchers concluded that the RMR measurement improved patient motivation and
confidence in following the recommended nutrition and activity plan. "Similar to other physiological parameters (i.e.,
cholesterol, blood pressure, glucose, etc.) that some clients would need to know to better manage a disease, the use of
RMR technology would provide a parameter (i.e., daily caloric intake goal) that may empower an individual to better manage body weight" [4].
Figure 2. Mean weight loss following 12 weeks of active treatment using the MedGem versus estimate [4].
How do you measure metabolism?
Metabolic rate is traditionally assessed using either direct or indirect calorimeter. Direct calorimetry
requires the precise measure of heat output using a large, expensive and technically complex whole body calorimeter.
Indirect calorimetry determines metabolic rate from oxygen consumption and is usually the ?Gold Standard? when assessing
metabolism. Indirect calorimeters are expensive $25,000-$50,000, require technical expertise to operate, and require routine
maintenance that can also be expensive.
Recently, Microlife Medical Home Solutions, Inc. harnessed revolutionary technology to manufacture the MedGem©
hand-held indirect calorimeter (Figure 3). The MedGem can measure oxygen consumption and determine a patient?s calorie needs.
Measuring oxygen consumption, rather than using estimates, allows healthcare providers to make the most accurate decisions for
their patient. With a simple breathing test of 10 minutes or less, a patient can now have their unique metabolism measured for
developing a personalized nutrition and activity plan that is best for their weight management goals.
Will my insurance company cover my metabolism measurement?
Medical Necessity must be established in order for the MedGem to be considered for reimbursement.
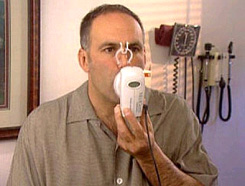
Figure 3. Individual RMR assessment using the MedGem? hand-held indirect calorimeter.
Individual payers develop their own criteria for medical necessity. The measurement may not be considered
medically necessary for weight management, and the coverage potential is higher if there is an underlying medical
need, such as a disease state.
Here is a list of conditions that The Center for Medicare Services (i.e. Medicare) has indicated as medically necessary for the procedure:
- Chronic airway obstruction (COPD)
- Shortness of breath
- Sleep Apnea
- Asthma
- Pulmonary Heart Disease
- Lung Cancer
Alternative diseases that may support medical necessity by private insurance companies include:
- Type 2 Diabetes
- Hypertension (High Blood Pressure)
- Hypercholesterolemia (High Cholesterol)
- Hypothyroidism
- Abnormal weigh gain
- Obesity
If you are overweight, you will likely need another medical condition such as the ones listed above.
Talk with your healthcare provider if the MedGem measurement is appropriate for you.
References:
1. Danforth, E., Jr., Dietary-induced thermogenisis: control of energy expenditure. Life Sci, 1981. 28(15-16): p. 1821-7.
2. Foster, G.D., et al., Resting energy expenditure, body composition, and excess weight in the obese. Metabolism, 1988. 37(5): p. 467-72.
3. ADA, Adult Weight Management Evidence-Based Nutrition Practice Guideline. 2007.
4. McDoniel, S.O., H.A. Nelson, and C.A. Thompson, Employing RMR technology in a 90 day weight control program. Obes Facts, 2008. 1(6): p. 298-304.
Source: 2008 ? Microlife Medical Home Solutions, Inc. All Rights Reserved. Microlife and WatchWT are registered trademarks of Microlife Corp.
MedGem is a registered trademark of Microlife Medical Home Solutions, Inc. PN: 995-0017-01-A
October 2009
|

